REPORTS
Diabetes Mellitus: Cognitive Effects and Treatment Opportunities
Presented by:Roger McIntyre, MD, FRCPC
Professor of Psychiatry and Pharmacology, University of Toronto, Toronto, Canada
Chairman and Executive Director, Brain and Cognition Discovery Foundation (BCDF), Toronto, Canada
Director, Depression and Bipolar Support Alliance (DBSA), Chicago, IL; USA
Patients with type 2 diabetes often struggle in areas related to cognition, motivation, reward, and sleep.1 Many subdomains of cognition are also affected and cognitive deficits have been shown in processing speed, executive function, attention, and memory.1 In a study assessing cognitive decline in patients with type 1 and type 2 diabetes compared to healthy controls, results demonstrated a decrease in information processing speed in patients with type 2 diabetes.2
In an effort to investigate depressive symptomatology and cognitive impairment as mediators of workplace productivity in patients with type 2 diabetes, a naturalistic, cross-sectional study was performed that included over 700 people.3 Participants had to work full- or part-time and meet the criteria for diabetes or prediabetes.3 Outcomes were based on the Endicott Workplace Productivity Scale (EWPS), Patient Health Questionnaire 9 items (PHQ-9), and the Perceived Deficits Questionnaire 5 items (PDQ-5).3 Findings demonstrated that self-rated depressive and cognitive symptoms were positively correlated with workplace impairment (absenteeism, mentally not present at work) among patients with or at risk type 2 diabetes, suggesting that cognition may be what is driving health outcomes and working effectiveness in individuals with type 2 diabetes.3
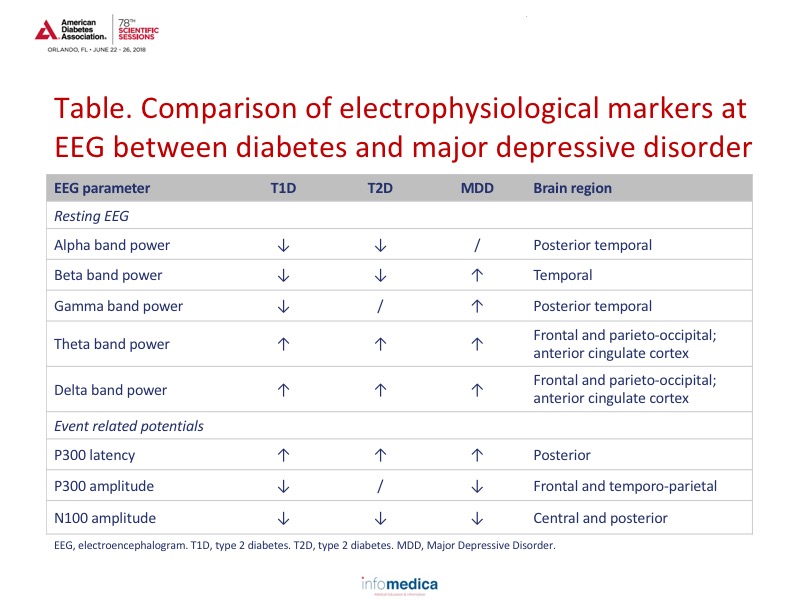
Recognizing that diabetes may cause changes in the brain, results from an electroencephalogram (EEG) in patients with type 1 and type 2 demonstrated a signature similar to what is found in major mood disorders such as Major Depressive Disorder (MDD); see Table.4
A study that focused on cognitive decline in patients who were at high risk or ultra-high risk for bipolar disorder also included the presence of overweight/obesity as a function of cognitive decline. Interestingly, results demonstrated that individuals at varying degrees of risk for bipolar disorder had a greater cognitive impairment as a function of co-existing overweight/obesity.5 These findings further strengthen the suggestion that obesity and cognitive decline are linked.5
Insulin adherence may also play a role in the reward system of the brain. In the normal brain, insulin and metabolic function are critical for brain neurobiology. As insulin is a monoamine oxidase, it reduces oxidative stress, which increases dopamine signaling and ultimately improves mood.6 In people with central insulin resistance, brain mitochondrial dysfunction (with increased oxidative stress) can lead to decreased dopamine signaling and subsequent anxiety and depressive-like behaviors.6
Intranasal insulin has been shown to increase cognition and improve functional brain connectivity.6,7 In a separate randomized, double-blind, controlled trial, intranasal insulin administration also improved measures of neurocognitive performance in euthymic adults with bipolar disorder. 8
Other commonly used antidiabetic agents have also shown improvements in cognitive function in patients suffering from mood disorders. For example, GLP-1 receptor agonists demonstrated action on the reward center in the brain. Liraglutide had beneficial effects on objective measures of cognitive function.9 Initial experimental studies on obese rats have also demonstrated amelioration of cognitive decline as well as attenuated brain apoptosis and brain inflammation with dapagliflozin (an SGLT2 inhibitor) and vildagliptin (a DPP4 inhibitor). 10
Key Messages
- Patients with type 2 diabetes have been shown to have declines in cognitive function.
- Overweight and obesity also appear to play a role in cognitive decline in patients with type 2 diabetes.
- Changes in brain physiology as a result of diabetes demonstrate a similar signature as mood depressive disorders.
- Intranasal insulin, GLP-1 receptor agonists, DPP4 inhibitors, and SGLT2 inhibitors have shown improvements in cognition when used as treatment for diabetes.
REFERENCES
Present disclosure: The presenter reported that he has received research and/or grants from Stanley Medical Research Institute, CIHR. China National Natural Research Foundation, Lundbeck, and Shire. In the past 2 years, he has received fees for speaking/consultation from Shire, Purdue, Otuska, Janssen-Ortho, Lundbeck, Pfizer, Neurocrine, Neuralstem, Sunovion, Takeda, and Allergan.
Written by: Debbie Anderson, PhD
Reviewed by: Marco Gallo, MD