REPORTS
Fast and Furious or Just Marketing Fiction? Expectations From New and Developing Rapid-Acting Insulins
Presented by:Tim Heise, MD
Profil, Neuss, Germany
The optimal goal for insulin therapy is to replicate physiological insulin levels normally found in the body, with rapid insulin action at meals and a slow decrease after meals.1 With the advent of rapid-acting insulin analogs, the question becomes whether they are truly fast-acting or not. While they do appear to work faster than human insulin, a 2-hour time to maximum effect2 does not seem “fast-acting” and perhaps reveals a marketing term as opposed to scientific validity.
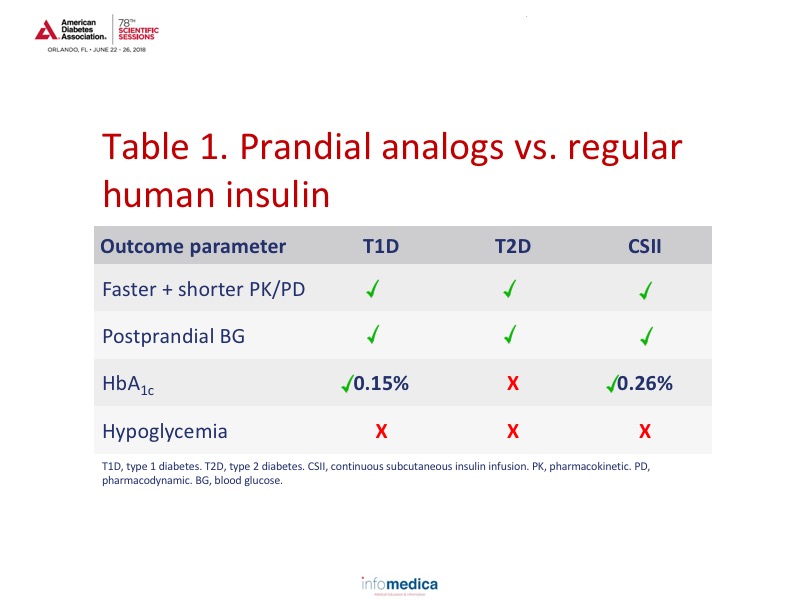
Prandial insulin analogs have shown advantages in patient with type 1 diabetes when compared with regular human insulin. Results based on a Cochrane Database review demonstrated a clear advantage of prandial insulin analogs over regular human insulin in HbA1c results.3 Unfortunately, these results were not duplicated in patients with type 2 diabetes.4 In a very small study (23 patients with type 2 diabetes patients and 10 controls), insulin aspart significantly reduced the area under the curve for postprandial hyperglycemia, preserved flow-mediated vasodilation, and improved endothelial function compared to regular insulin.5 Another study demonstrated a partial reversal of myocardial perfusion abnormalities with the use of an insulin analog through the improvement of glucose control, when compared to regular insulin.6 However, this was also a very small study (n = 20) and more information is needed before making any conclusions. When reviewing data for analog use in continuous glucose monitoring/insulin pumps, lispro demonstrated significant improvements in glycated hemoglobin over regular human insulin and was preferred by patients.7 All in all, prandial analogs appear to show advantages over regular human insulin as can be seen in Table 1.
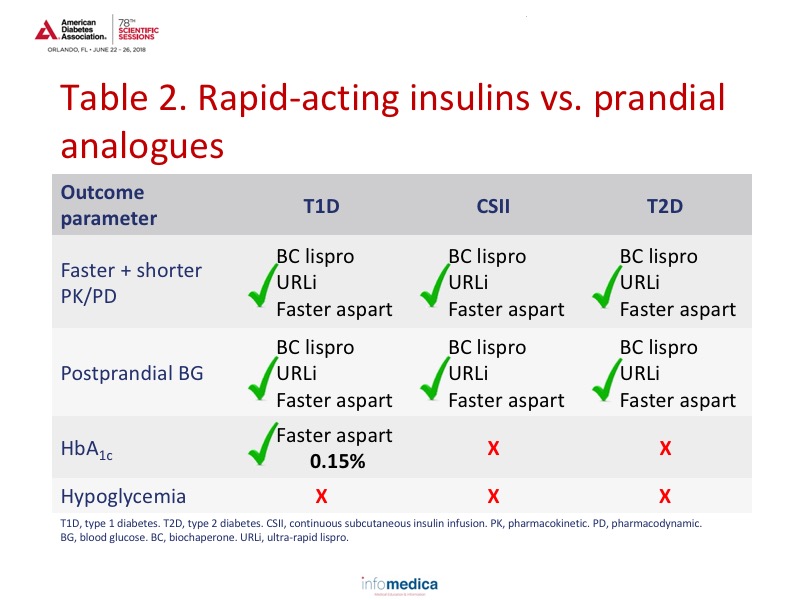
Three rapid-acting insulins that are appearing are biochaperone lispro, ultra-rapid lispro (URLi), and faster aspart. Biochaperone lispro and URLi have faster “on” times than lispro, while faster aspart is quite similar in timing to insulin aspart.8-10 All of these new formulations have also shown improvements in postprandial blood glucose levels in both patients with type 1 and type 2 diabetes.11-13 When reviewing its clinical efficacy and application, fast-acting insulin aspart effectively improved HbA1c values in patients with type 1 diabetes and demonstrated superior postprandial glucose over insulin aspart.14 Faster aspart was also non-inferior to insulin aspart for basal-bolus regimens as for HbA1c levels, with no differences in hypoglycemia rates, body weight, and safety data.15 When used in insulin pumps, faster aspart had slightly higher results in HbA1c but had more favorable results with interstitial glucose and postprandial glucose findings.16 Overall, the new rapid-acting insulins have modest advantages over prandial analogues which are summarized in Table 2.
Key messages
- The optimal goal for insulin therapy is to replicate physiological insulin levels normally found in the body.
- Prandial insulin analogues have shown advantages over regular human insulin in type 1 diabetes.
- New rapid-acting insulins have shown benefits in pharmacokinetic/pharmacodynamic data and postprandial blood glucose.
REFERENCES
Present disclosure: The presenter reported that he has received research funds from Adocia, Boehringer Ingelheim, Dance Pharmaceuticals, Eli Lilly, Johnson & Johnson, Medimmune, MSD, Mylan, Nordic Bioscience, Novo Nordisk, Poxel, Roche Diagnostics, Saniona, Sanofi, Senseonics, and Zealand Pharma. He has also been a member of advisory panels for Novo Nordisk and Mylan. He has received speaker honoraria and travel grants from Dexcom, Eli Lilly, Mylan, Novo Nordisk, Sanofi, and Zealand Pharma.
Written by: Debbie Anderson, PhD
Reviewed by: Marco Gallo, MD