REPORTS
Management of Hyperglycemia in Type 2 Diabetes–Draft ADA/EASD Consensus Report 2018
Presented by:Peter Rossing, MD
Steno Diabetes Center Copenhagen Gentofte, Denmark
Deborah J. Wexler, PhD, MSc
Massachusetts General Hospital Boston, MA; USA
Walter Kernan, MD
Yale School of Medicine, New Haven, CT; USA
Geltrude Mingrone, MD PhD
Catholic University of The Sacred Heart, Rome, Italy
David D’Alessio, MD
Duke University, Durham, NC; USA
Chantal Mathieu, MD, PhD
KU Leuven, Leuven, Belgium
The report addresses the approaches to glycemic management in adults with type 2 diabetes, with the goal of reducing complications and maintaining quality of life. The key points which have been emphasized, for the draft of the ADA/EASD consensus report 2018, include the following:
- Greater focus on lifestyle interventions, with increased emphasis on weight loss and obesity management, including metabolic surgery
- Greater focus on patient-related issues and self-management
- Preferred choices of anti-hyperglycemic agents driven by new evidence from cardiovascular outcome trials
- Consideration of areas of major clinical need
The report focuses on how to achieve each patient’s individualized glycemic target by taking into account patient factors, preferences, and increasing choice of therapies available for glycemic control.
The draft consensus report pays special attention to assessing key patient characteristics and preferences, which are central to therapeutic decision making. The four characteristics of focus include:
- Comorbidities–atherosclerotic cardiovascular disease (ASCVD)/chronic kidney disease (CKD)
- Clinical characteristics–age, HbA1c, weight
- Motivation/depression
- Cultural and socio-economic context.
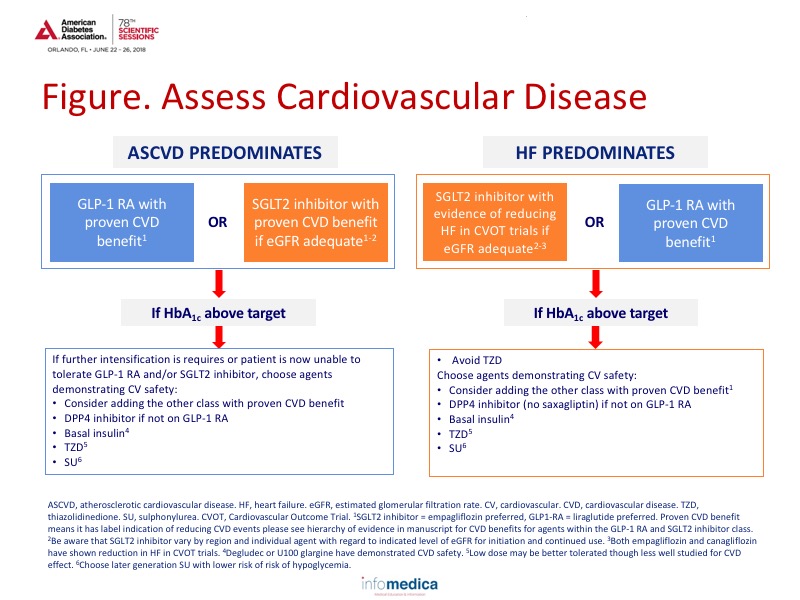
The most important step for physicians is to assess the presence of CVD and to further quantify whether ASCVD or congestive heart failure (CHF) predominates (see Figure 1). In type 2 diabetes patients with established ASCVD, SGLT2 inhibitors (empagliflozin preferred, otherwise canagliflozin) or GLP-1 receptor agonists (GLP-1 RAs: liraglutide preferred, otherwise semaglutide, or exenatide LAR) with proven cardiovascular benefits are recommended. If CHF predominates, physicians should consider the use of an SGLT2 inhibitor as part of the treatment strategy.
Physicians must also consider the presence of CKD. In these patients with high cardiovascular risk, GLP-1 RAs and SGLT2 inhibitors are recommended, albeit with dose reductions for some medications. In fact, several of these medications have demonstrated renal and cardiovascular benefits and should be considered as part of treatment.
Medical nutrition therapy (MNT) is still an important part of diabetes management. It is defined as education and support to help patients adopt healthy eating patterns and it includes two main components: diet quality and calorie restriction. The quality of the diet is important as no single ratio of proteins, carbohydrates, or fat is right for every patient. Instead, food with known health benefits (e.g., fruit and vegetables) should be emphasized. Furthermore, some diet patterns (e.g., the Mediterranean diet) may help reduce hyperglycemia.
Physical activity has been shown effective in reducing HbA1c levels by ~0.6% and should be encouraged in all patients with type 2 diabetes. Naturally, more exercise is better and has additional health benefits such as reduced ASCVD risk factors, reduced fall risk, reduced weight, and increased bone density.
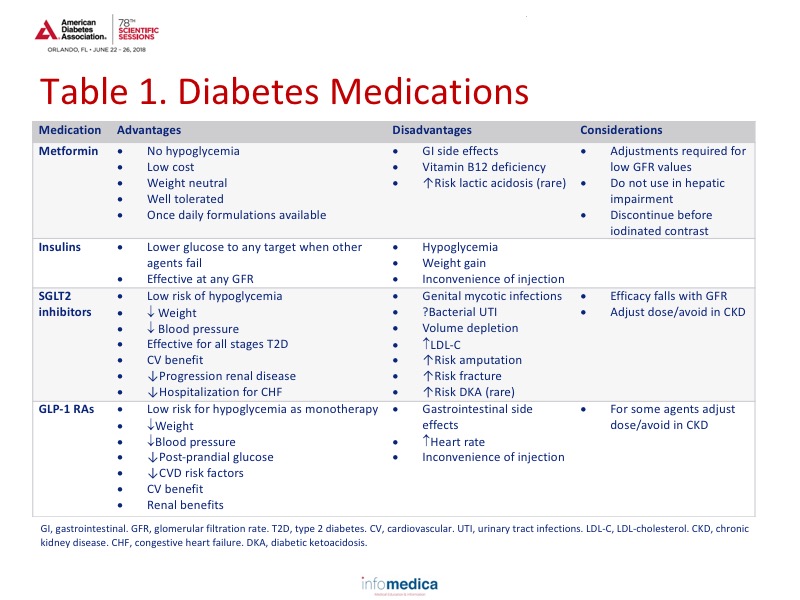
Medications are another option for the management of patients with type 2 diabetes. Antidiabetic drugs have a number of benefits and limitations. The most commonly used medications can be viewed in more depth in Table 1.
Not included in Table 1 are five classes of antidiabetic drugs that are rarely used in clinical practice: meglitinides, ɑ-glucosidase Inhibitors, bile acid sequestrants, dopamine agonists, and amylin mimetics.
Metabolic surgery may also be indicated in patients with type 2 diabetes with failed non-surgical therapy for obesity. Its main contraindications are untreated eating disorders, untreated depression/psychosis, substance abuse, and inability to follow nutritional advice. There are numerous benefits to metabolic surgery including high rates of diabetes remission, improved glycemic control, reduction in use of glucose lowering medications, and marked weight reduction. Main risks (within 2 years) include surgical complications, insufficient weight loss, and late metabolic complications (iron deficiency).
Metabolic surgery, which is to be considered as a very effective salvage therapy, is recommended for adults with type 2 diabetes and a body mass index (BMI) ≥40 kg/m2 (BMI ≥37.5 kg/m2 in people of Asian ancestry) regardless of level of glycemic control, and with BMI 35.0-39.9 kg/m2 (32.5-37.4 kg/m2 in people of Asian ancestry) when hyperglycemia is inadequately controlled despite lifestyle and optimal medical therapy.
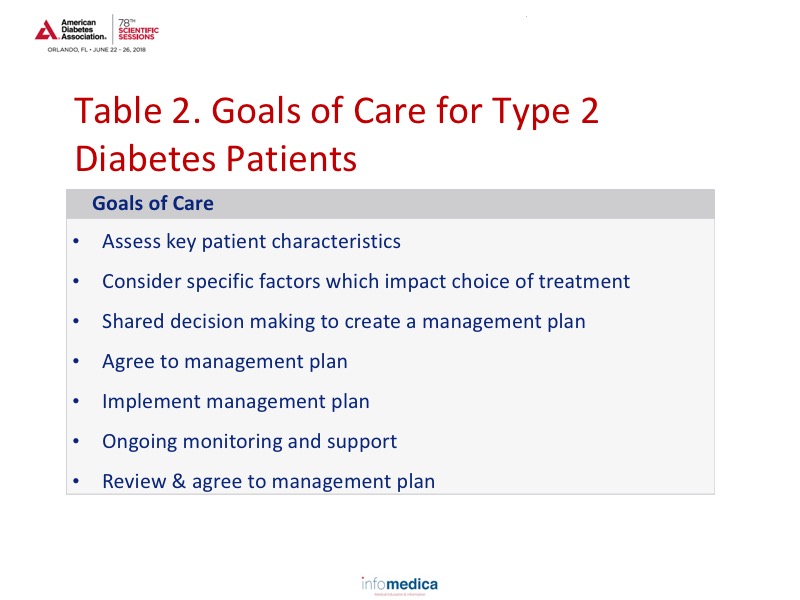
The ADA/EASD consensus has developed a “Goals of Care” plan that focuses on preventing complications and optimizing quality of life through a number of steps (see Table 2).
Metformin continues to be the foundational therapy along with comprehensive lifestyle management in patients with type 2 diabetes. However, physicians should consider the stepwise addition of antihyperglycemic medication (to be generally preferred to initial combination therapy) by determining the presence of ASCVD, CHF, or other comorbidities, weight loss, the need to minimize hypoglycemia, and and any other needs including whether cost is an issue. Recommendations and treatment goals are provided for each step in the process.
In patients without ASCVD or CHF risk and high HbA1c, SGLT-2 inhibitors, GLP-1 RAs, thiazolidinediones, and DPP4 inhibitors are all preferred options, but each have specific characteristics. Suggestions are also provided based on costs.
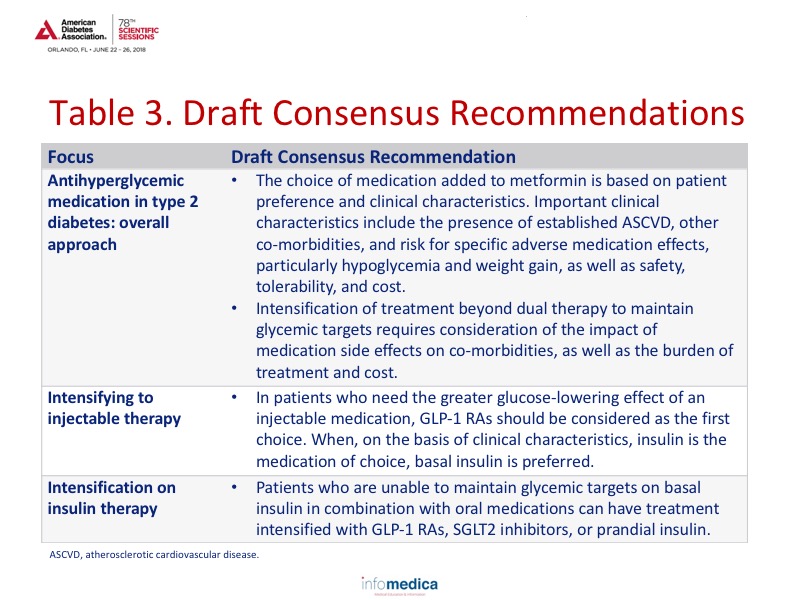
Intensification to injectable therapies is also reviewed, based on high HbA1c despite dual or triple oral therapy. Incorporation of basal insulin and BD or TDS premixed insulin is recommended in specific instances along with active discussions with diabetes specialists as needed. Review Table 3 for a summary of the Draft consensus statements.
Key messages
- The presence or absence of ASCVD and congestive heart failure needs to be considered in patients with type 2 diabetes.
- An individualized program of medical nutritional therapy should be offered to all patients.
- Overweight and obese patients with diabetes should be advised of the health benefits of weight loss and encouraged to engage in a program of intensive lifestyle management.
- Increasing physical activity improves glycemic control and should be encouraged in all patients with type 2 diabetes.
- Metabolic surgery is a recommended treatment option for adults with type 2 diabetes and a BMI ≥40 kg/m2 regardless of level of glycemic control, and with BMI 35.0-39.9 kg/m2 when hyperglycemia is inadequately controlled despite lifestyle and optimal medical therapy.
- The overall diabetes regimen should be based on patient preference and clinical characteristics.
- Access, treatment cost, and insurance coverage should all be considered when selecting antihyperglycemic medications.
REFERENCES
Present disclosure: All of the presenters, except those listed below, have reported no disclosures.
Peter Rossing: the presenter reported that he has received consultant and/or speaking fees from AbbVie, Astellas, Astra Zeneca, Bayer, Boehringer Ingelheim, Bristol-Myers Squibb, Eli Lilly, MSD, Novo Nordisk and Sanofi Aventis. He has received research grants from AbbVie, Astra Zeneca, and Novo Nordisk and is a stock/shareholder for Novo Nordisk.
Geltrude Mingrone: the presenter reported that she is a consultant for Novo Nordisk, Fractyl Inc, and Johnson & Johnson.
David D’Alessio: the presenter reported that he was involved in advisory boards for Eli Lilly, Intarcia, and Novo Nordisk. He has also received research support from Merck and Eli Lilly.
Chantal Mathieu: the presenter reported that she was involved in advisory boards for Astra Zeneca, Boehringer Ingelheim, Bristol-Myers Squibb, Eli Lilly, Hanmi Pharmaceuticals, Intrexon, Janssen Pharmaceuticals, Mannkind, Medtronic, Merck Sharp & Dohme, Novartis, Novo Nordisk, Pfizer, Roche Diagnostics, Sanofi, and UCB. She has been on the speaker’s bureau for Astra Zeneca, Boehringer Ingelheim, Eli Lilly, Merck Sharp & Dohme, Novartis, Novo Nordisk, and Sanofi. She has also received research support from Abbott, Eli Lilly, Intrexon, Merck Sharp & Dohme, Novartis, Novo Nordisk, Roche Diagnostic, and Sanofi.
Written by: Debbie Anderson, PhD
Reviewed by: Marco Gallo, MD